The next in our "Best of the Month" series comes from May 20, 2011:
 |
| Lester S. Adelman, MD |
I was recently sent this 1992 essay written by Dr. Lester S. Adelman,
retired neuropathologist at Tufts New England Medical Center. It
amusingly illustrates the anonymity in which we pathologists toil:
Pathologists spend their time in the figurative,
and sometimes literal bowels of the hospital.
Even those of us who specialize in the pathology
of the brain occupy this nether region. The
patients who benefit from our brilliant diagnoses
are often as little aware of us as they are of
the hospital laundry.
This life of anonymity has its rewards. Frozen sections
are only rarely done on nights and weekends, and straightforward
cases are disposed of quickly. The intellectual and
visual pleasures of the job are great. Every once in a while,
however, we are reminded of the fact that we have given up
a part of doctoring, the part that has to do with knowing the
gratitude of the patients whom we help.
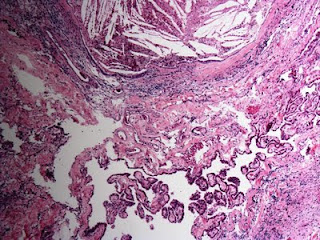
Some years ago, in the era before CT scans and MRIs,
a patient was admitted to our hospital with a brain tumor.
Preoperative radiologic diagnoses in those days were based
on angiography, and this patient's angiogram strongly suggested
a glioblastoma multiforme. The patient was given the
bad news, and a biopsy was done to confirm the diagnosis.
The surgeons also thought the tumor was a glioblastoma,
but when I looked at the frozen section, I discovered the
tumor was clearly a meningioma. With this diagnosis, the
surgeons were able to find a plane of dissection around the
tumor and remove it completely.
I was happy with the outcome and thought I had accepted
the fact that the patient would never know my part .
in it. It was not long after that I was to come face-to-face
with the shortcomings of my chosen medical specialty.
A week later I was at a conference with the neurosurgeons
when I noticed that one of the residents was wearing
an expensive new wristwatch. A moment later I noticed that
a senior neurosurgeon had a similar watch on his wrist. A
quick check of the audience revealed that they all had new
watches!
"What's going on?" I asked.
"You remember Mr. X, the patient with the meningioma?
He's a jeweler, and he was so happy he didn't have
a glioblastoma that he gave us all new watches."
"How about me?" I whined. "I'm the one who cured
him. If it weren't for me, you would have quit, thinking he
had a glioblastoma."
The physicians smiled graciously and conceded this was
probably the case.
Years have passed, and despite the advances in imaging,
my neurosurgical colleagues continue to consult me about
diagnoses. But when I want to know what time it is I still
consult my Timex.

 Now that it's winter and our noses and sinuses are being dried out by our heating systems, many of us turn to neti pots (also known as 'nose bidets'). The illustrious J. Clay Goodman, MD, neuropathologist at Baylor, just sent me an article from The Houston Chronicle warning people to use distilled, bottled, or boiled water. Officials in Louisiana are investigating whether a 51-year-old woman and a 20-year-old man both contracted the brain-eating amoeba Naegleria fowleri after using tap water in their neti pots. The disease, while rare, is most commonly contracted after inhaling
water from a lake, pond or river. If investigators confirm the two
victims died after using tap water from a neti pot it will be the first
time the disease has been contracted from tap water.
Now that it's winter and our noses and sinuses are being dried out by our heating systems, many of us turn to neti pots (also known as 'nose bidets'). The illustrious J. Clay Goodman, MD, neuropathologist at Baylor, just sent me an article from The Houston Chronicle warning people to use distilled, bottled, or boiled water. Officials in Louisiana are investigating whether a 51-year-old woman and a 20-year-old man both contracted the brain-eating amoeba Naegleria fowleri after using tap water in their neti pots. The disease, while rare, is most commonly contracted after inhaling
water from a lake, pond or river. If investigators confirm the two
victims died after using tap water from a neti pot it will be the first
time the disease has been contracted from tap water.